What Intervention Does the Nurse Perform to Provide a Relaxed Environment for Labor?
Pain Management
Kitty Cashion
Pain is an unpleasant, complex, highly individualized phenomenon with sensory and emotional components. Pregnant women ordinarily worry about the pain they volition experience during labor and birth and well-nigh how they volition react to and deal with that pain. A variety of nonpharmacologic and pharmacologic methods can assistance the woman or the couple cope with the pain of labor. The methods selected depend on the situation, the availability, and the preferences of the woman and her health intendance provider. This affiliate volition talk over sources of intrapartum pain and factors that touch women's response to pain. It will also describe nonpharmacologic and pharmacologic methods unremarkably used for hurting relief.
Pain During Labor and Birth
Neurologic Origins
The hurting and discomfort of labor have two origins—visceral and somatic. During the first stage of labor, uterine contractions crusade cervical dilation and effacement. Uterine ischemia (decreased claret menstruum and therefore local oxygen deficit) results from compression of the arteries supplying the myometrium during uterine contractions. Pain impulses during the first stage of labor are transmitted via the T10 to T12 and L1 spinal nerve segments and accessory lower thoracic and upper lumbar sympathetic nerves. These nerves originate in the uterine torso and cervix (Blackburn, 2013).
The pain from distention of the lower uterine segment, stretching of cervical tissue as information technology effaces and dilates, pressure level and traction on next structures (eastward.k., uterine tubes, ovaries, ligaments) and nerves, and uterine ischemia during the first stage of labor is visceral pain. It is located over the lower portion of the belly. Referred hurting occurs when pain that originates in the uterus radiates to the abdominal wall, lumbosacral area of the back, iliac crests, gluteal area, thighs, and lower back (Blackburn, 2013; Zwelling, Johnson, and Allen, 2006).
During most of the offset phase of labor, the woman ordinarily has discomfort only during contractions and is free of pain betwixt contractions. Some women, especially those whose fetus is in a posterior position, experience continuous contraction-related low back hurting, even in the interval between contractions. As labor progresses and pain becomes more intense and persistent, women get fatigued and discouraged, frequently experiencing difficulty coping with contractions (Creehan, 2008; Zwelling, Johnson, and Allen, 2006).
During the 2nd stage of labor, the adult female has somatic pain, which is often described as intense, precipitous, burning, and well localized. This pain results from:
As women concentrate on the work of bearing down to give birth to their baby, they may report a decrease in hurting intensity (Blackburn, 2013; Creehan, 2008). Pain impulses during the 2nd stage of labor are transmitted via the pudendal nerve through S2 to S4 spinal nervus segments and the parasympathetic system (Blackburn, 2013).
Pain experienced during the third stage of labor and the afterpains of the early on postpartum menstruum are uterine, similar to the hurting experienced early in the first stage of labor. Areas of pain during labor are shown in Fig. 14-1.
Expression of Hurting
Pain results in physiologic effects and sensory and emotional (affective) responses. During childbirth, hurting gives rise to identifiable physiologic effects. Sympathetic nervous arrangement activity is stimulated in response to intensifying hurting, resulting in increased catecholamine levels. Blood pressure and centre rate increase. Maternal respiratory patterns change in response to an increment in oxygen consumption. Hyperventilation, sometimes accompanied past respiratory alkalosis, can occur as pain intensifies and more rapid, shallow breathing techniques are used during contractions. Pallor and diaphoresis may be seen. Gastric acidity increases, and nausea and vomiting are mutual in the active and transition phases of the outset phase of labor. Placental perfusion may decrease, and uterine activity may diminish, potentially prolonging labor and affecting fetal well-being.
Certain emotional (affective) expressions of hurting oftentimes are seen. Such changes include increasing anxiety with lessened perceptual field, writhing, crying, groaning, gesturing (paw clenching and wringing), and excessive muscular excitability throughout the body.
Factors Influencing Pain Response
Hurting during childbirth is unique to each woman. How she perceives or interprets that hurting is influenced by a variety of physiologic, psychologic, emotional, social, cultural, and environmental factors (Zwelling, Johnson, and Allen, 2006).
Civilisation
The population of pregnant women reflects the increasingly multicultural nature of order in the United States. As nurses care for women and families from a variety of cultural backgrounds, they must accept knowledge and understanding of how culture mediates pain. Although all women expect to experience at least some pain and discomfort during childbirth, information technology is their civilisation and religious conventionalities organization that determines how they will perceive, interpret, and reply to and manage the pain. For example, women with potent religious beliefs often take hurting as a necessary and inevitable part of bringing a new life into the world (Callister, Khalaf, Semenic, et al., 2003). An understanding of the beliefs, values, expectations, and practices of various cultures will narrow the cultural gap and help the nurse appraise the laboring woman's pain experience more than accurately. The nurse can then provide advisable, culturally sensitive care by using hurting relief measures that preserve the adult female'south sense of control and cocky-conviction (see Cultural Competence box). Recognize that although a woman'due south beliefs in response to pain may vary according to her cultural background, it may not accurately reflect the intensity of the hurting she is experiencing. Assess the adult female for the physiologic effects of hurting, and listen to the words she uses to describe the sensory and affective qualities of her pain (encounter Community Focus box).
Anxiety
Anxiety is usually associated with increased pain during labor. Mild anxiety is considered normal for a woman during labor and birth. However, excessive anxiety and fear cause more than catecholamine secretion, which increases the stimuli to the encephalon from the pelvis considering of decreased blood menses and increased muscle tension. This activeness, in turn, magnifies pain perception. Thus as anxiety and fear heighten, muscle tension increases, the effectiveness of uterine contractions decreases, the experience of discomfort increases, and a cycle of increased fear and feet begins (Blackburn, 2013). Ultimately this bicycle will slow the progress of labor. The woman's confidence in her ability to cope with hurting will be diminished, potentially resulting in reduced effectiveness of the hurting relief measures being used.
Gate-Control Theory of Hurting
Even especially intense pain stimuli can at times be ignored. This is possible because certain nerve cell groupings within the spinal string, brainstem, and cerebral cortex accept the ability to modulate the hurting impulse through a blocking mechanism. This gate-control theory of hurting helps explain the manner hypnosis and the hurting relief techniques taught in childbirth preparation classes piece of work to relieve the pain of labor. Co-ordinate to this theory, pain sensations travel along sensory nervus pathways to the brain simply only a limited number of sensations, or letters, tin travel through these nerve pathways at one time. Using distraction techniques such every bit massage or stroking, music, focal points, and imagery reduces or completely blocks the capacity of nerve pathways to transmit pain. These distractions are idea to work past endmost down a hypothetic gate in the spinal cord, thus preventing hurting signals from reaching the brain. The perception of pain is thereby diminished.
In addition, when the laboring woman engages in neuromuscular and motor activity, action inside the spinal cord itself further modifies the manual of hurting. Cognitive work involving concentration on breathing and relaxation requires selective and directed cortical action that activates and closes the gating mechanism as well. Every bit labor intensifies, more circuitous cognitive techniques are required to maintain effectiveness. The gate-control theory underscores the need for a supportive birth setting that allows the laboring adult female to relax and utilise various higher mental activities.
Condolement
Although the predominant medical approach to labor is that information technology is painful and the pain must be removed, an alternative view is that labor is a natural process and women tin feel condolement and transcend the discomfort or pain to reach the joyful result of birth. Having needs and desires met promotes a feeling of comfort. The nearly helpful interventions in enhancing comfort are a caring nursing approach and a supportive presence.
Support
Electric current evidence indicates that a adult female's satisfaction with her labor and birth experience is determined by how well her personal expectations of childbirth were met and the quality of support and interaction she received from her caregivers (Box 14-1). In addition, satisfaction is influenced by the caste to which she was able to stay in control of her labor and to participate in determination making regarding her labor, including the pain relief measures to be used (Albers, 2007; Zwelling, Johnson, and Allen, 2006).
The value of the continuous supportive presence of a person (e.1000., doula, childbirth educator, family unit member, friend, nurse, or partner) during labor who provides physical comforting, facilitates communication, and offers data and guidance to the woman in labor has long been known. Emotional support is demonstrated by giving praise and reassurance and carrying a positive, calm, and confident demeanor when caring for the adult female in labor (Creehan, 2008). It is interesting to note that research findings have concluded that a more positive effect is achieved when the continuous support is provided by people who are not infirmary staff members (Hodnett, Gates, Hofmeyr, et al., 2011).
Environs
The quality of the environment tin can influence pain perception and the laboring woman's ability to cope with her pain. Environment includes the individuals present (due east.g., how they communicate, their philosophy of care including a belief in the value of nonpharmacologic pain relief measures, practice policies, and quality of support) and the concrete infinite in which the labor occurs (Creehan, 2008; Zwelling, Johnson, and Allen, 2006). Women usually prefer to be cared for by familiar caregivers in a comfortable, homelike setting. The environment should be safe and individual, allowing a adult female to feel costless to be herself as she tries out different comfort measures. Stimuli such as lite, noise, and temperature should be adjusted co-ordinate to her preferences. The environment should have space for motility and equipment such as birth balls. Comfortable chairs, tubs, and showers should be readily bachelor to facilitate participation in a variety of nonpharmacologic pain relief measures. The familiarity of the environment tin can be enhanced by bringing items from habitation such equally pillows, objects for a focal point, music, and DVDs.
Nonpharmacologic Pain Management
The alleviation of pain is important. Commonly information technology is not the amount of hurting the woman experiences but whether she meets the goals she set for herself to cope with the pain that influences her perception of the birth experience as skilful or bad. The observant nurse looks for clues to the adult female'southward desired level of control in the management of pain and its relief.
Nonpharmacologic measures are frequently unproblematic and condom, have few if any major adverse reactions, are relatively inexpensive, and can be used throughout labor. In addition, they provide the woman with a sense of control over her childbirth as she makes choices virtually the measures that are best for her. During the prenatal period, she should explore a variety of nonpharmacologic measures. Techniques she unremarkably finds helpful in relieving stress and enhancing relaxation (east.g., music, meditation, massage, warm baths) may be very constructive every bit components of a plan for managing labor pain. The woman should be encouraged to communicate to her health intendance providers her preferences for relaxation and hurting relief measures and to actively participate in their implementation.
Many of the nonpharmacologic methods for relief of discomfort are taught in different types of prenatal training classes, or the woman or couple may accept read various books and magazine articles on the field of study in accelerate. Many of these methods require exercise for best results (due east.g., hypnosis, patterned breathing and controlled relaxation techniques, biofeedback), although the nurse may utilize some of them successfully without the woman or couple having prior knowledge (e.g., boring-paced breathing, massage and touch on, effleurage, counterpressure). Women should be encouraged to endeavor a diverseness of methods. Oft nonpharmacologic methods are used in combination with pharmacologic methods, particularly as labor progresses.
With the increasing use of epidural analgesia, nurses may exist less probable to encourage women to use nonpharmacologic measures, in role because these methods may be viewed as more complex and time consuming than monitoring a woman receiving an epidural. In addition, new nurses may not accept had the opportunity to develop skill in the implementation of these methods. Information technology is imperative that perinatal nurses develop a commitment to and expertise in using a diversity of nonpharmacologic pain relief strategies in society for women in labor to be comfortable using them. Although research data to support the effectiveness of many of these nonpharmacologic measures are limited, there are sufficient reports of their benefits from women and health care providers to recommend that nurses encourage their apply (Creehan, 2008). The analgesic effect of many nonpharmacologic measures is comparable to or even superior to opioids that are administered parenterally (Box 14-two).
Childbirth Grooming Methods
The childbirth education movement began in the 1950s. Today virtually health care providers recommend or offer childbirth preparation classes for expectant parents. Historically, popular childbirth methods taught in the U.s.a. were the Dick-Read method, the Lamaze (psychoprophylaxis) method, and the Bradley (hubby-coached childbirth) method. Although these three organizations go on to exist, they are now less focused on a "method" approach. Rather, women are assisted to develop their birth philosophy and inner knowledge and then choose from a variety of skills to use to cope with the labor procedure. Many childbirth educators teach a diversity of techniques that originated in several different organizations or publications. Women are encouraged to choose the techniques that work best for them.
Gaining popularity are methods developed and promoted by Birthing From Within, Birthworks, Association of Labor Assistants and Childbirth Educators (ALACE), Childbirth and Postpartum Professional Association (CAPPA), and HypnoBirthing, to name a few. These methods offer classes and other services that focus on fostering a woman's confidence in her innate ability to requite nascence. The woman or couple are helped to recognize the uniqueness of their pregnancy and childbirth experience.
Relaxation and Breathing Techniques
Relaxation
Relaxation or reduction of trunk tension is a technique suggested by virtually all childbirth pedagogy organizations. Learning relaxation in childbirth instruction classes can aid couples with the stresses of pregnancy, childbirth, and adjustment to parenting and tin can be a form of stress management throughout life (Fig. 14-ii). Prove suggests that relaxation may better the management of labor pain (Jones, Othman, Dowswell, et al., 2012). Relaxation is ideally combined with action such as walking, slow dancing, rocking, and position changes that aid the baby rotate through the pelvis. Rhythmic move stimulates mechanoreceptors in the brain, which decreases pain perception.
The nurse tin can assistance the woman past providing a serenity and relaxed environment, offering cues as needed, and recognizing signs of tension (e.yard., frowning, change in tone of voice, clenching of fists). A relaxed surroundings for labor is created past controlling sensory stimuli (e.g., low-cal, noise, temperature) and reducing interruptions. Nurses should remain at-home and unhurried in their arroyo and sit rather than stand at the bedside whenever possible (Creehan, 2008).
Breathing Techniques
Different approaches to childbirth preparation stress varying animate techniques to provide lark, thereby reducing the perception of pain and helping the adult female maintain control throughout contractions. In the kickoff stage of labor, such breathing techniques tin can promote relaxation of the abdominal muscles and thereby increase the size of the abdominal cavity. This lessens discomfort generated by friction betwixt the uterus and abdominal wall during contractions. Because the muscles of the genital surface area also become more relaxed, they do non interfere with fetal descent. In the second phase, animate is used to increase intestinal pressure and thereby help in expelling the fetus. Breathing also can be used to relax the pudendal muscles to prevent precipitate expulsion of the fetal head (Fig. 14-3).
For couples who have prepared for labor by practicing relaxing and animate techniques, a simple review with occasional reminders may be all that is necessary to help them forth. For those who accept had no preparation, instruction and exercise in simple breathing and relaxation techniques tin can be given early on in labor and often is surprisingly successful. Nurses can too model breathing techniques and exhale in synchrony with the adult female and her partner. Motivation is high and readiness to acquire is enhanced by the reality of labor (meet Critical Thinking Case Study).
Various animate techniques can be used for controlling hurting during contractions (Box 14-3). The nurse needs to determine what, if any, techniques the laboring couple know earlier giving them educational activity. Uncomplicated patterns are more hands learned. Paced breathing is most associated with prepared childbirth and includes slow-paced, modified-paced, and patterned-paced breathing (pant-blow) techniques. Each labor is unlike, and nursing back up includes assisting couples to adjust breathing techniques to their individual labor feel.
All patterns brainstorm with a deep, relaxing, cleansing breath to "greet the contraction" and stop with another deep breath exhaled to "gently blow the contraction away." These deep breaths ensure adequate oxygen for female parent and baby and signal that a contraction is beginning or has ended. As the breath is exhaled, respiratory and voluntary muscles relax (Creehan, 2008). In general, irksome-paced animate is performed at approximately half the adult female's normal breathing rate and is initiated when she can no longer walk or talk through contractions. The woman should take no fewer than three or 4 breaths per minute. Slow-paced breathing aids in relaxation and provides optimum oxygenation. The adult female should go along to utilise this technique for as long as it is effective in reducing the perception of pain and maintaining control. Equally contractions increase in frequency and intensity, the woman frequently needs to change to a more circuitous breathing technique, which is shallower and faster than her normal rate of breathing but should not exceed twice her resting respiratory rate. This modified-paced breathing pattern requires that she remain alert and concentrate more fully on breathing, thus blocking more painful stimuli than the simpler slow-paced breathing pattern (Perinatal Didactics Assembly, 2008 [www.birthsource.com]).
The nigh difficult time to maintain control during contractions comes during the transition phase of the first stage of labor, when the cervix dilates from 8 cm to 10 cm. Even for the woman who has prepared for labor, concentration on breathing techniques is difficult to maintain. Patterned-paced (pant-blow) animate is suggested during this phase. Information technology is performed at the same charge per unit as modified-paced breathing and consists of panting breaths combined with soft blowing breaths at regular intervals. The patterns may vary (i.e., pant, pant, pant, pant, accident [4 : i design] or pant, pant, pant, blow [three : 1 pattern]) (Perinatal Instruction Associates, 2008). An undesirable reaction to this type of breathing is hyperventilation. The woman and her support person must exist aware of and scout for symptoms of the resultant respiratory alkalosis: lightheadedness, dizziness, tingling of the fingers, or circumoral numbness. Respiratory alkalosis may be eliminated by having the adult female breathe into a newspaper purse held tightly around her mouth and nose. This enables her to rebreathe carbon dioxide and supplant the bicarbonate ions. The adult female also can exhale into her cupped hands if no bag is available. Maintaining a breathing rate that is no more than twice the normal rate will lessen chances of hyperventilation. The partner can help the woman maintain her breathing charge per unit with visual, tactile, or auditory cues.
Equally the fetal head reaches the pelvic floor, the woman may feel the urge to push and may automatically brainstorm to exert downward pressure level by contracting her abdominal muscles. During second-stage pushing, the woman should find a breathing pattern that is relaxing and feels good to her and is safe for her infant. Any regular or rhythmic breathing that avoids prolonged breath belongings during pushing should maintain a expert oxygen flow to the fetus (Perinatal Instruction Associates, 2008).
The woman can control the urge to push by taking panting breaths or past slowly exhaling through pursed lips (as though blowing out a candle or blowing up a balloon). This type of animate can exist used to overcome the urge to push when the cervix is not fully prepared (east.g., less than 8 cm dilated, not retracting) and to facilitate a boring nascency of the fetal caput.
Touch and Massage
Touch and massage accept been an integral part of the traditional care process for women in labor. A variety of massage techniques accept been shown to be safety and effective during labor (Gilbert, 2011; Zwelling, Johnson, and Allen, 2006).
Impact can be equally simple as belongings the woman's hand, stroking her body, and embracing her. When using touch to communicate caring, reassurance, and business, it is important that the woman'due south preferences for touch (east.grand., who can touch her, where they tin touch her, and how they can touch her) and responses to bear on exist determined. A woman with a history of sexual abuse or certain cultural beliefs may be uncomfortable with bear upon. Touch likewise tin can involve very specialized techniques that require manipulation of the human energy field.
Therapeutic touch (TT) uses the concept of energy fields within the body called prana. Prana are thought to be scarce in some people who are in pain. TT uses laying-on of hands by a especially trained person to redirect energy fields associated with pain. Enquiry has demonstrated the effectiveness of TT to enhance relaxation, reduce feet, and relieve hurting (Aghabati, Mohammadi, and Pour Esmaiel, 2010); however, little is known about the use or effectiveness of TT for relieving labor pain.
Head, hand, dorsum, and human foot massage may exist very effective in reducing tension and enhancing comfort. Some evidence suggests that massage may meliorate direction of labor hurting (Jones, Othman, Dowswell, et al., 2012). Hand and human foot massage may exist especially relaxing in avant-garde labor when hyperesthesia limits a woman's tolerance for touch on other parts of her body. The woman and her partner should be encouraged to experiment with different types of massage during pregnancy to determine what might feel best and be most relaxing during labor.
Application of Oestrus and Common cold
Warmed blankets, warm compresses, heated rice bags, a warm bath or shower, or a moist heating pad tin can enhance relaxation and reduce pain during labor. Estrus relieves musculus ischemia and increases blood flow to the area of discomfort. Heat application is effective for dorsum hurting acquired past a posterior presentation or general backache from fatigue.
Common cold awarding such equally cold cloths, frozen gel packs, or ice packs applied to the back, the chest, and/or the face during labor may be effective in increasing condolement when the woman feels warm. They also may exist applied to areas of musculoskeletal pain. Cooling relieves pain past reducing the muscle temperature and relieving musculus spasms (Creehan, 2008). Even so, a woman's culture may make the use of cold during labor unacceptable.
Heat and cold may be used alternately for a greater effect. Neither heat nor common cold should be applied over ischemic or anesthetized areas considering tissues can be damaged. One or ii layers of cloth should be placed betwixt the skin and a hot or cold pack to prevent damage to the underlying integument (run across Disquisitional Thinking Case Written report).
Acupressure and Acupuncture
Acupressure and acupuncture can exist used in pregnancy, in labor, and postpartum to relieve pain and other discomforts. Pressure, oestrus, or cold is applied to acupuncture points chosen tsubos. These points take an increased density of neuroreceptors and increased electrical conductivity. Acupressure is said to promote circulation of blood, the harmony of yin and yang, and the secretion of neurotransmitters, thus maintaining normal body functions and enhancing well-being (Tournaire and Theau-Yonneau, 2007). Acupressure is best practical over the peel without using lubricants. Pressure is usually applied with the heel of the hand, fist, or pads of the thumbs and fingers (Fig. 14-4). Tennis balls or other devices besides may be used. Pressure is applied with contractions initially so continuously as labor progresses to the transition phase at the end of the first stage of labor (Tournaire and Theau-Yonneau, 2007). Synchronized breathing by the caregiver and the woman is suggested for greater effectiveness. Acupressure points are found on the neck, the shoulders, the wrists, the lower dorsum including sacral points, the hips, the area below the kneecaps, the ankles, the nails on the pocket-sized toes, and the soles of the feet. Prove is bereft to back up the effectiveness of acupressure equally a method of pain relief during labor (Smith, Collins, Cyna, et al., 2006).
Acupuncture is the insertion of fine needles into specific areas of the trunk to restore the flow of qi (energy) and to decrease hurting, which is thought to be obstructing the period of free energy. Effectiveness may exist attributed to the amending of chemical neurotransmitter levels in the body or to the release of endorphins as a consequence of hypothalamic activation. Acupuncture should be washed by a trained certified therapist, and arranging to accept a qualified and credentialed acupuncture provider available during labor and birth may exist challenging (Hawkins and Bucklin, 2012). Current evidence indicates that acupuncture may be beneficial for relief of labor pain; however, further written report is indicated (Hawkins and Bucklin, 2012; Jones, Othman, Dowswell, et al., 2012).
H2o Therapy (Hydrotherapy)
Bathing, showering, and jet hydrotherapy (whirlpool baths) with warm h2o (e.1000., at or below body temperature) are nonpharmacologic measures that can promote comfort and relaxation during labor (Fig. 14-6). The warm h2o stimulates the release of endorphins, relaxes fibers to shut the gate on pain, promotes ameliorate circulation and oxygenation, and helps soften the perineal tissues. Virtually women discover immersion in water to be soothing, relaxing, and comforting. While immersed, they may find it easier to allow get and allow labor to take its class (Gilbert, 2011). Some prove suggests that immersion in water may meliorate management of labor pain (Jones, Othman, Dowswell, et al., 2012).
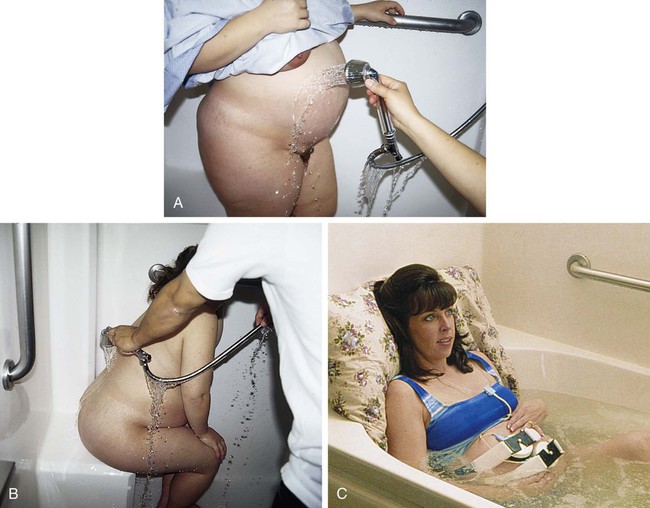
Earlier initiating hydrotherapy measures, agency policy should be consulted to make up one's mind if the approval of the laboring woman'south principal health intendance provider is required and if criteria demand to exist met in terms of the status of the maternal and fetal unit (e.g., stable vital signs and fetal heart rate [FHR] and pattern, and stage of labor). To reduce the risk of a prolonged labor, hydrotherapy is usually initiated when the woman is in active labor, at approximately five cm. It is at this time that she may be getting discouraged and volition welcome the change that hydrotherapy offers. Remember to preserve her modesty because she may be shy near the exposure of her body when getting into a tub or shower (Creehan, 2008).
In improver to pain relief and relaxation, hydrotherapy offers other benefits. If a woman is having "back labor" as the effect of an occiput posterior or transverse position, assuming a hands-and-knees or a side-lying position in the tub enhances spontaneous fetal rotation to the occiput anterior position as a issue of increased buoyancy. Because less endeavour is needed to change positions while in the water, women are encouraged to presume upright positions and to alter positions more frequently, facilitating the progress of their labors and helping them cope with labor-associated stressors (Stark, Rudell, and Haus, 2008).
When hydrotherapy is in employ, FHR monitoring is done by Doppler, fetoscope, or wireless external monitor (see Fig. 14-6, C). Placement of internal electrodes is contraindicated for jet hydrotherapy. There is no limit to the time women can stay in the bathroom, and often they are encouraged to stay in it equally long every bit desired. However, nigh women use jet hydrotherapy for 30 to 60 minutes at a fourth dimension. During the bathroom, if the woman's temperature and the FHR increment, if the labor procedure becomes less effective (e.m., slows or becomes too intense), or if relief of pain is reduced, the woman tin can come up out of the bathroom and render at a later time. Repeated baths with occasional breaks may be more effective in relieving pain in long labors than extended amounts of time in the water. The temperature of the h2o should be maintained at 36° to 37° C (96.8° to 98.half dozen° F) with the water covering the adult female's abdomen to gain maximum effect from the hydrostatic pressure and buoyancy of the h2o. Her shoulders should remain out of the h2o to facilitate the dissipation of heat (Creehan, 2008).
The American Academy of Pediatrics Committee on Fetus and Newborn has expressed concerns about actual birthing in water because of the lack of research demonstrating its safety. There are rare only reported instances of asphyxia or infection that have occurred during or equally a result of underwater nativity. This group believes that underwater nativity should be considered an experimental procedure, performed but after informed parental consent has been obtained (Hawkins and Bucklin, 2012).
Using a shower provides comfort through the application of heat as the handheld shower head is directed to areas of discomfort (run across Fig. 14-half-dozen, A and B). The passenger vehicle or partner can participate in this comfort measure by holding and directing the shower caput.
Aromatherapy
Aromatherapy uses oils distilled from plants, flowers, herbs, and trees to promote wellness and to treat and residue the mind, body, and spirit. These essential oils are highly full-bodied, complex essences and are mixed with lotions or creams earlier they are applied to the skin (eastward.g., for a back massage). Certain essential oils can tone the uterus, encourage contractions, reduce pain, salvage tension, diminish fear and feet, and enhance the feeling of well-beingness. Lavender, rose, and jasmine oils can promote relaxation and reduce pain. Rose oil also acts as an antidepressant and uterine tonic, whereas jasmine oil strengthens contractions and decreases feelings of panic in add-on to reducing pain. Essential oils of bergamot or rosemary tin be diffused or used in a massage oil to salve exhaustion (Gilbert, 2011; Tournaire and Theau-Yonneau, 2007; Walls, 2009). Oils may besides be used by adding a few drops to a warm bath, to warm water used for soaking compresses that tin can be applied to the body, or to an aromatherapy lamp to vaporize a room. Drops of essential oils can exist put on a pillow or on a woman'south brow or palms or used every bit an ingredient in creating massage oil (Simkin and Bolding, 2004; Walls, 2009; Zwelling, Johnson, and Allen, 2006). Sure odors or scents can evoke pleasant memories and feelings of love and security. Every bit a outcome, it would be helpful for a adult female to choose the scents that she will use (Trout, 2004). There is insufficient evidence to back up the effectiveness of aromatherapy for pain relief in labor although its utilise has elicited promising results (Jones, Othman, Dowswell, et al., 2012; Smith, Collins, Cyna, et al., 2006; Zwelling, Johnson, and Allen, 2006).
Music
Music, recorded or live, can provide a distraction, enhance relaxation, and lift spirits during labor, thereby reducing the woman'due south level of stress, anxiety, and perception of pain. It can be used to promote relaxation in early labor and to stimulate movement as labor progresses. Music can help create a more than relaxed temper in the birth room, leading to a more relaxed approach by health intendance providers (Creehan, 2008; Zwelling, Johnson, and Allen, 2006). Women should be encouraged to prepare their musical preferences in accelerate and to bring a CD player or MP3 thespian (e.g., iPod) to the hospital or birthing center. They should cull familiar music that is associated with pleasant memories, which can too facilitate the process of guided imagery. Utilize of a headset or earphones may increment the effectiveness of the music because other sounds will be close out. Live music provided at the bedside by a support person may be very helpful in transmitting energy that decreases tension and elevates mood. Irresolute the tempo of the music to coincide with the rate and rhythm of each animate technique may facilitate proper pacing. Prove is insufficient to back up the effectiveness of music as a method of pain relief during labor. Further research is recommended (Smith, Collins, Cyna, et al., 2006).
Merely gilt members can continue reading. Log In or Register to continue
Source: https://nursekey.com/pain-management-3/#:~:text=A%20relaxed%20environment%20for%20labor,possible%20(Creehan%2C%202008).